Are you aware that January is Cervical Cancer Awareness Month?
If you’re from the tri-state area, you might have heard the famous phrase, “Forget About it.” Pronounced “Fuhgeddaboutit” by locals. But please don’t. You just can’t.
Because even though we’ve seen remarkable progress in improving statistics around the diagnosis and death associated with Cervical Cancer, people are still needlessly dying from it. That means we’re losing our beloved mothers, sisters, daughters, aunts, best friends, grandparents, and trans brothers, sons, fathers, and uncles.
Thanks to the Pap (Smear) test and the Human Papillomavirus (HPV) test, which can be done alone or together (co-testing), lives are being saved, often before cancer even develops.
In addition, HPV vaccines are protecting patients against the high-risk types of HPV responsible for causing 90% of cervical cancers. But our work is far from finished.
In 2024, the estimate for new cases of cervical cancer in the U.S was 13,820 with about 4,360 estimated deaths. Here’s the surprising fact: Cervical Cancer can be detected, and easily treated—and cured—if caught early enough. And that’s important because precancers develop slowly and often cause no symptoms.
While HPV and Pap Smear Tests have been routinely used for detection, there’s a new alternative in town and a new way to put the power in patients’ hands.
The latest FDA-approved test offers patients either a swab or brush to enable self-collection of a vaginal specimen to screen for HPV right in the doctor’s office or in a healthcare setting. So, people can skip the standard physician-administered pelvic exam and go straight to the test. Now that’s different—and easier!
Still, there are barriers to screening. Some people live in remote areas, making it difficult to routinely check in with their healthcare professionals, while others might not be aware they need to prioritize testing, and for some testing simply falls off their radar.
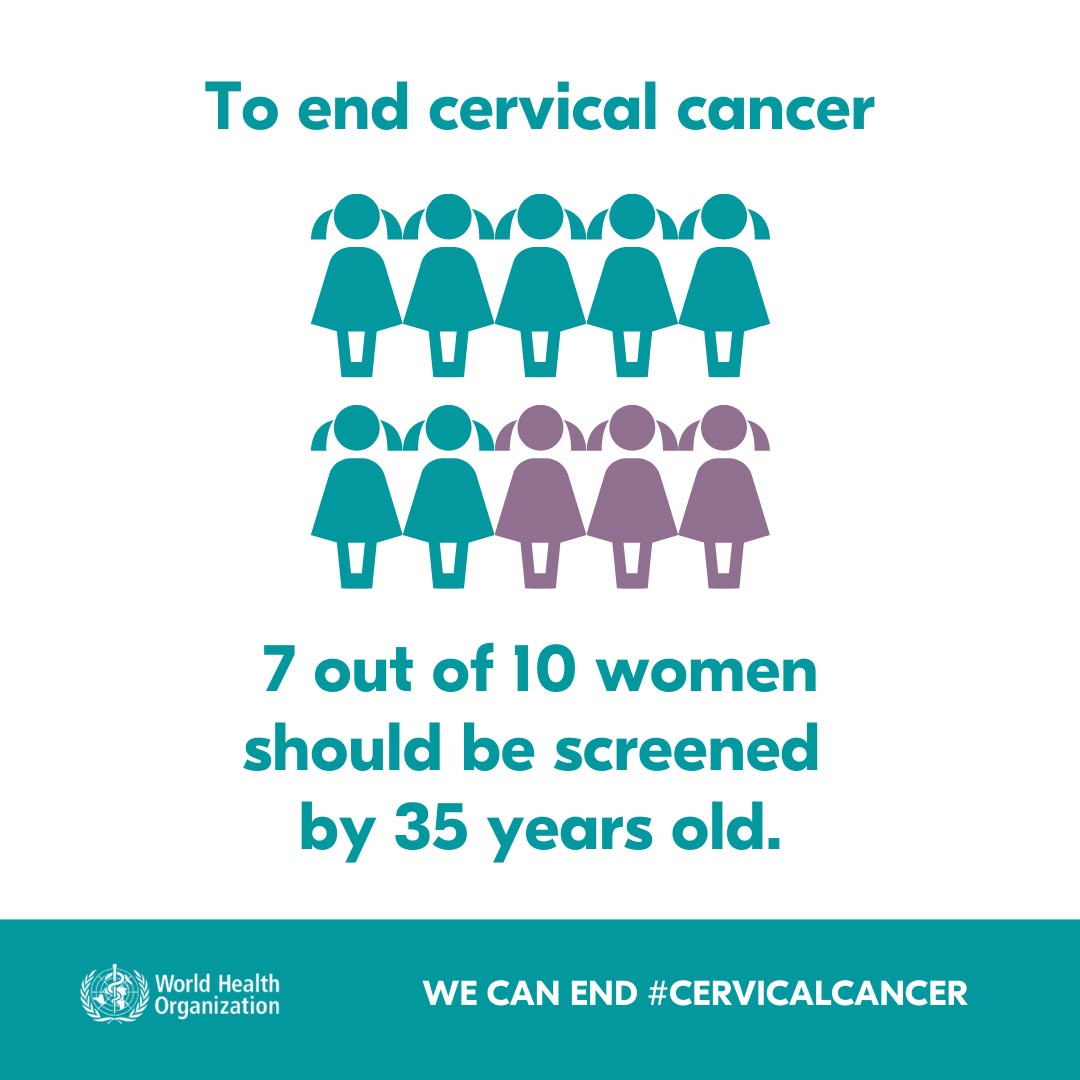
If we aim to wipe out cervical cancer by the year 2030, an ambitious global movement put into action by the World Health Assembly in 2020, we’ll need to amplify awareness about screening and prevention.
The US Preventive Services Task Force (USPSTF) is in the process of updating their recommendations on Cervical Cancer Screening. A summary of the current recommendation calls for screening every 3 years with cervical cytology (Pap Smear Test) in women ages 21 to 29 and then every 5 years with -clinician or -patient-collected high risk HPV primary screening in women ages 30 to 65.
And while there are other organizations with different recommendations, there is one thing everyone agrees on; regular screening—however it’s done—saves lives.
So, in honor of Cervical Cancer Awareness Month and joining the effort to wipe out the disease by 2030, don’t forget to nudge your mom to get tested. Nudge your daughter. Nudge your spouse. And, of course, don’t forget about yourself. We can change the reality of Cervical Cancer. Let’s do this!
If your brand team would like to hear about our agency’s unique process and learn how we instill a different reality into messaging, branding, and strategy, contact Jon or Hoon at RRx. Let’s talk.
References:
- Cancer Stat Facts: Cervical Cancer. National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Accessed January 24, 2025. https://seer.cancer.gov/statfacts/html/cervix.html.
- Screening for Cervical Cancer. U.S. Centers for Disease Control and Prevention. Accessed January 24, 2025. https://www.cdc.gov/cervical-cancer/screening/index.html.
- Human Papillomavirus (HPV). U.S. Centers for Disease Control and Prevention. August 20, 2024. Accessed January 24, 2025. https://www.cdc.gov/hpv/vaccines/index.html#:~:text=The%20vaccine%20is%20safe%20and,the%20cervix%20in%20young%20women
- Cervical Cancer Causes, Risk Factors, and Prevention. National Cancer Institute. Updated. August 2, 2024. Accessed January 24, 2025. https://www.cancer.gov/types/cervical/causes-risk-prevention.
- Cervical Cancer Elimination Initiative. World Health Organization. Accessed January 24, 2025. https://www.who.int/initiatives/cervical-cancer-elimination-initiative
- Berg, Sara, MS. What doctors wish patients knew about cervical cancer prevention. AMA. Jan 13, 2023. Accessed January 24, 2025. https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-cervical-cancer-prevention.
- Reynolds, S. FDA Approves HPV Tests That Allow for Self-Collection in a Health Care Setting. National Cancer Institute. July 24, 2024. Accessed January 24, 2025. https://www.cancer.gov/news-events/cancer-currents-blog/2024/fda-hpv-test-self-collection-health-care-setting.
- Cervical Cancer Screening. Draft Recommendation Statement. US Preventive Services Task Force. Update in Progress. December 4, 2024. Accessed January 24, 2025. https://www.uspreventiveservicestaskforce.org/uspstf/draft-update-summary/cervical-cancer-screening-adults-adolescents
- Cervical Cancer Screening. National Cancer Institute. Updated May 17, 2024. Accessed January 24, 2025. https://www.cancer.gov/types/cervical/screening#:~:text=The%20human%20papillomavirus%20(HPV)%20test,untreated%E2%80%94turn%20into%20cervical%20cancer.

